Graves Orbitopathy (GO) or Thyroid Eye Disease (TED) is an autoimmune disease that involves inflammation of the tissues of the orbit (eye muscles, fatty and connective tissues) and the tissues around the eye. Typical initial symptoms are swelling of the eyelids, retraction of the eyelids, pressure pain behind the eye, watery eyes and sensitivity to light, especially early in the morning.
GO most commonly occurs in Graves’ disease, but ocular symptoms may also appear in normal or decreased thyroid function (e.g Hashimoto’s thyroiditis). In most cases, EO appears simultaneously with thyroid disease, but may precede or follow thyroid disorders or surgical thyroidectomy.
Why does the orbital inflammation arise?
B Graves’ disease is an autoimmune disease that targets the body’s own tissues (thyroid gland, eyes and skin) with the body’s own so-called autoantibodies (auto=self). In the case of eye involvement, the fibroblasts (connective tissue cells) behind the eye are attacked, which leads to a remodeling and expansion of the connective and fatty tissues as well as the eye muscle.

What are the typical complaints or symptoms?
Patients with active GO complain most about: pressure pain behind the eye, painful eye movements, protruding eyes, change in appearance (e.g. an anxious look), watery and burning, dry eyes, photophobia and double vision. In severe cases: drastically reduced visual acuity and/or color vision disorders..
Quality of life is also severely affected in many patients due to the limitations in daily life which can lead to serious mood swings, even depression.
The crucial factors for the management of GO are: early recognition, accurate grading ( assessment of inflammatory activity) and an optimally tailored patient-oriented multidisciplinary therapy. Close cooperation with endocrinologists, thyroid surgeons and oral and maxillofacial surgeons is essential.
Management of Graves Orbitopathy:
1) Thyroid function adjustments after determination of thyroid hormone and antibody levels.
2) Lubricants (drops during the day, ointment at night).
3) Lifestyle changes: e.g a drastic reduction/cessation of smoking
4) Selenium as a dietary supplement
5) In moderate or severe active GO: intravenous steroid therapy, in special cases also combined with radiotherapy
6) In severe EO, acute orbital decompression (orbital dilation) is rarely necessary to relieve the optic nerve
7) When the GO is inactive (this process can take several months) the restorative surgeries can be: Exophthalmos reduction by decompression (orbital expansion) and/or strabismus and/or eyelid surgery can be carried out.
Strabismus surgery in Graves orbitopathy
In GO, two specific eye muscles, the inferior and the medial rectus muscles, are most commonly affected by inflammation, leading to distracting double vision. In strabismus surgery, the stiffened, fibrotic eye muscles are recessed (weakened) in order to restore the balance of the muscles.
The surgery is carried out under general anesthesia.
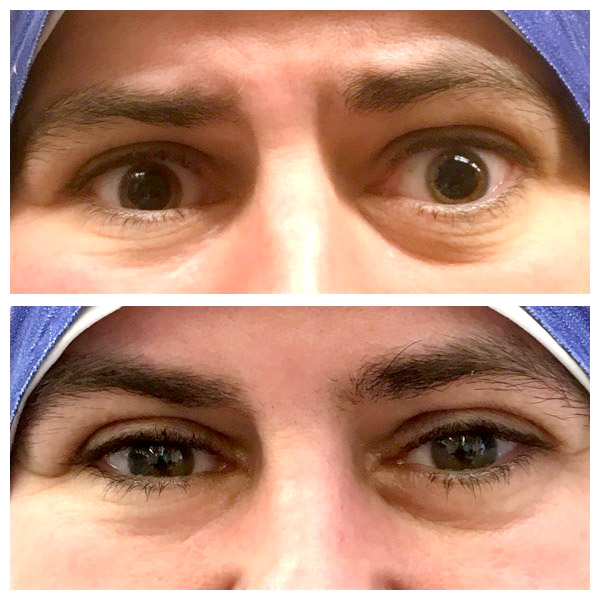
Specific eyelid surgery for Graves Orbitopathy:
Since the eyelid lifting muscle is also shortened by the inflammation and -as a result of which – the eye is no longer completely covered-, the surface of the eye dries out. Furthermore, the facial expression is strongly altered by the retraction of the upper eyelid, sometimes the eyelids are also noticeably swollen due to the expansion of the fatty tissue. Furthermore, the lacrimal gland is enlarged and protrudes. During the eyelid surgery, the upper eyelid is lengthened, the excess fatty tissue is removed and the lacrimal glands are repositioned in their original position. This operation can be performed under local anesthesia or under general anesthesia.